
Health disparities are all around us. We see them in our friends, family members, neighbors, colleagues, and — for clinicians — patients. Many of us have experienced them in our own lives.
Hispanic Americans are more than twice as likely as their white counterparts to be uninsured, leading to meaningful gaps in care. Black Americans are more likely to die from heart disease than other ethnic or racial groups. Maternal mortality rates are estimated to be ~3.5x higher in Black women than white women. These are just a small handful of the countless examples of healthcare disparities that Americans experience daily.
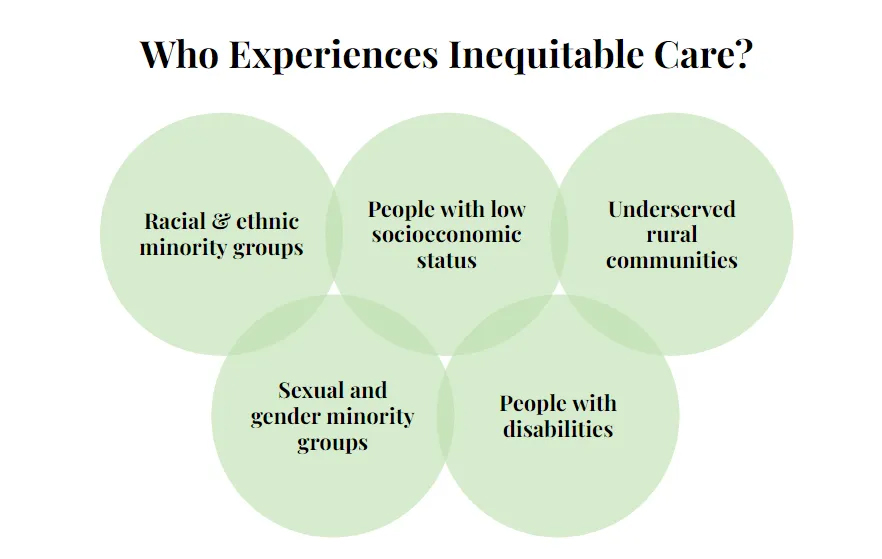
Health inequities fall into two categories: access and outcomes. Access includes barriers like cost and proximity to care. Outcomes involve receiving subpar care due to factors like bias, difficulty navigating the system, or a lack of cultural competency. As a result, racial and ethnic minorities, people with low socioeconomic status, underserved rural communities, sexual and gender minority groups, people with disabilities and others experience adverse discrepancies in their care. What we’re talking about is Social Determinants of Health: “The conditions in which people are born, live, learn, work, play, worship, and age impact their health, their quality of life, and the quality of care they receive.”
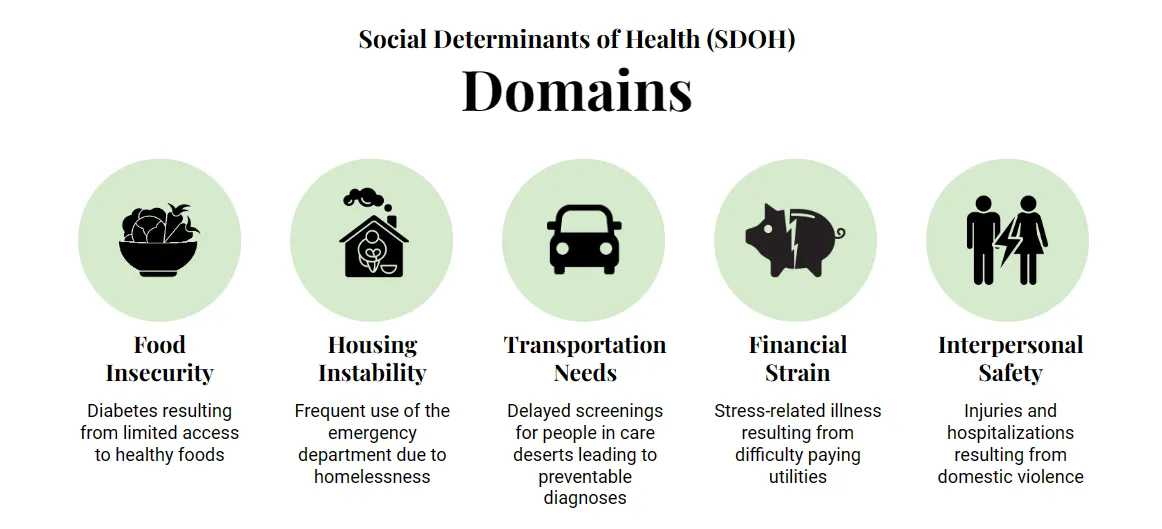
Social determinants of health fall under five distinct domains. Here are just a few examples:
- Food insecurity: for instance, people lacking access to healthy food options may be more vulnerable to conditions like diabetes due to dietary limitations.
- Housing instability: folks who are unhoused may have higher instances of emergency department visits due to the challenges and dangers inherent to living without stable shelter.
- Transportation needs: in rural areas, limited access to transportation can delay critical health screenings for preventable diseases, allowing conditions to advance beyond the point of effective treatment.
- Financial strain: difficulty paying utilities can be a significant burden, contributing to an increased likelihood of stress-related illnesses like high blood pressure and heart disease.
- Interpersonal safety: for example, victims of domestic violence may have a heightened risk of hospitalization due to sustained injuries.
Social determinants of health influence the entire continuum of care and are pervasive across the U.S.: in the graphic below from The Commonwealth Fund, health systems are scored for performance by race / ethnicity. Almost universally white patients score the highest, with a range of discrepancies across Black, Hispanic, Asian and American Indian patients.

Altogether, social determinants of health are estimated to account for as much as 80% of health outcomes.
So, how do we change these statistics, and create a more equitable health system? This is where digital health comes in.
The NIH defines digital health as “the use of information and communications technologies in medicine and other health professions to manage illnesses and health risks and to promote wellness.” To many, the term digital health sounds like an oxymoron — after all, only so much of healthcare can be delivered in a fully virtual environment. However, digital health solutions don’t seek to replace traditional healthcare, but rather to complement, support, and expand the capabilities of our healthcare system. Think of it as 2 + 2 = 5.
Digital health companies use different forms of technology to improve access to and quality of care, create efficiencies in healthcare workflows, and make care more personal and affordable for patients. Wearables like Fitbit and Oura that were initially sold as consumer fitness and sleep trackers are now being used as clinical tools to enable remote patient monitoring and catch care incidents earlier. Solutions ranging from apps on our mobile phones to mobile clinics in our neighborhoods are helping us bring better quality care to care deserts. The pandemic finally got patients, physicians and regulators comfortable with telemedicine, which greatly expands who, where and how often patients can access care. And, clinicians are seeing changes to their workflows, and can expect technologies like artificial intelligence to be directly integrated into the EHR through solutions like Tali AI to take more administrative work off their plates.
The digital health market has grown from $350B in 2019 to an estimated $600B this year. A significant portion of this market growth has been driven by VC funding, with half a billion in funding for solutions that target SDOH in 2021 alone.

At TMV, we believe that digital health companies possess a number of unique characteristics that help them tackle the challenges of healthcare inequity. Many of these companies are still relatively small startups compared to the industry giants, so they are able to move quickly and pivot to meet regulatory changes and customer needs in real-time. They are digitally native, powered by the latest technology from the start, rather than integrating new technology into an existing solution with a legacy tech stack familiar to a large workforce. They have an outsider’s perspective, and can draw learnings from spaces like fintech, consumer products, advertising, and education to bring fresh ideas to the space. And, of course, there is funding for these ambitious, sometimes unorthodox approaches and shoot-for-the-moon ideas.
To illustrate what this looks like in practice, below are a few examples of unique domains within health equity where digital health companies are building innovative solutions to close gaps.
- As we shift from fee-for-service to value-based health care, digital companies are working in partnership with payers to build new models of care delivery from the ground up. Cityblock Health built a value-based primary care solution for Medicaid patients, powered by a proprietary, fully integrated technology solution. Oak Street Health has a similar model for the Medicare population. And Millie has designed a midwifery-led care model that, in partnership with OBGYNs and a technology-enabled patient experience, is delivering superior maternal health outcomes.
- To support the transition to value-based care, companies like Pearl Health offer population health software that allows providers to visualize their panels, increase response time to patient inquiries, and track performance metrics used to calculate savings. Meanwhile, Wellvana’s approach is more hands-on and intensive, as they partner with practices to take on 100% of downside risk and 75% of shared savings while implementing their population health software and other operational improvements.
- To improve underlying health, companies are working with payers to expand and improve coverage for new types of treatment. “Food as medicine” startups like Swap Health and NourishedRX provide nutrition counseling for low and middle income patients, along with engaging benefits like rebates for buying healthier groceries, healthy meal delivery, and more.
- Today, only ~75% of providers accept Medicaid, in part due to lower reimbursement rates and challenges in getting reimbursed. To expand access for Medicaid patients, companies are building tools like telemedicine platforms and remote patient monitoring devices to help Medicaid providers better serve their patient base, and workflow tools to help Medicaid providers manage their patients’ medical and social needs. For example, Twentyeight Health is a digital pharmacy that focuses on Medicaid reimbursements and engaging a Medicaid audience rather than primarily serving the commercial market.
- And, in order to improve outcomes, companies are helping Medicaid patients get the most out of their plans. Often, Medicaid patients don’t fully utilize the services and benefits available to them for a number of reasons, including a lack of digestible information, trust in the system, and clear lines of communication. Fabric Health creates a bridge between hard-to-reach Medicaid patients and plans, setting up in laundromats to find and enroll the most vulnerable patients and help them access and engage with their plans.
- These companies and more are using technologies, tools and differentiated mechanisms to power their innovative models.

Digital companions powered by AI and self-serve content answer basic, frequently asked patient questions to empower patients and save clinicians time (see: Roon). Remote patient monitoring devices allow physicians to oversee patients between visits and drive earlier interventions when necessary. Community spaces like laundromats, community centers and barbershops help build trust and deliver care in familiar, accessible spaces. Digital health companies are supplementing providers with subclinical labor like community health workers and health coaches to expand care in supply-constrained specialties. Translation and health literacy tools help to ensure more equity at the point of care. The list goes on.
Digital health companies are driving innovation to close equity gaps, but they cannot do it alone. To create an impactful product, they must build for their audience: design and test product with users early and often, build a diverse team that reflects their customer base, and prioritize trust-building with their users. And, they must find the right partners to scale: collaborate with community organizations and institutions to meet folks where they are, and work with providers, health systems, and payers to reach patients and deliver better, more affordable care at scale.
This type of work is what drew me to investing: the opportunity to use technology and innovative business models to provide more equitable care for patients, everywhere. The innovative solutions that have already come to the forefront, and the passionate, brilliant founders with whom we get to partner make me more optimistic about the future of healthcare.
By Emma Silverman, Principal at TMV
*This post is based on a keynote speech delivered by Emma Silverman at the Advocate Health Heart Institute’s 17th annual Prevention to Cure Symposium in Chicago on February 7, 2024.
**For more insights on fostering equity through digital health innovation, I recommend reading Rock Health’s thoughtfully written, “A Lens on Health Equity in Digital Health: Unlocking the Innovation Opportunity” and checking out their Advancing Health Equity Innovation in Digital Health initiative.